|
even for people lucky enough to work for organizations that offer affordable insurance plans, the difference in employer-negotiated rates for those plans is also eye-opening. I was working for a 10k+ person joint, but we opted for my wife's insurance for both of us because she was working for the largest employer in one of the largest counties in the US and they threw their weight around with insurance companies. We saved a couple grand a year on co-pays and witholdings. just fuckin nationalize it already
|
|
|
|

|
| # ? May 5, 2024 07:15 |
|
captainbananas posted:even for people lucky enough to work for organizations that offer affordable insurance plans, the difference in employer-negotiated rates for those plans is also eye-opening. I was working for a 10k+ person joint, but we opted for my wife's insurance for both of us because she was working for the largest employer in one of the largest counties in the US and they threw their weight around with insurance companies. We saved a couple grand a year on co-pays and witholdings. I have a pretty good plan, we have no kids, and I'm paying $172.80 every two weeks for premiums. My wife takes a medication that's $28K every two months, I figure if they ever stop covering that we're hosed lol
|
|
|
|
Buck Turgidson posted:ok here's a fun exercise. open your search engine of choice and look up "usa average cost covid-19 hospital stay" we dont. that would cost money
|
|
|
|
|
|
|
|
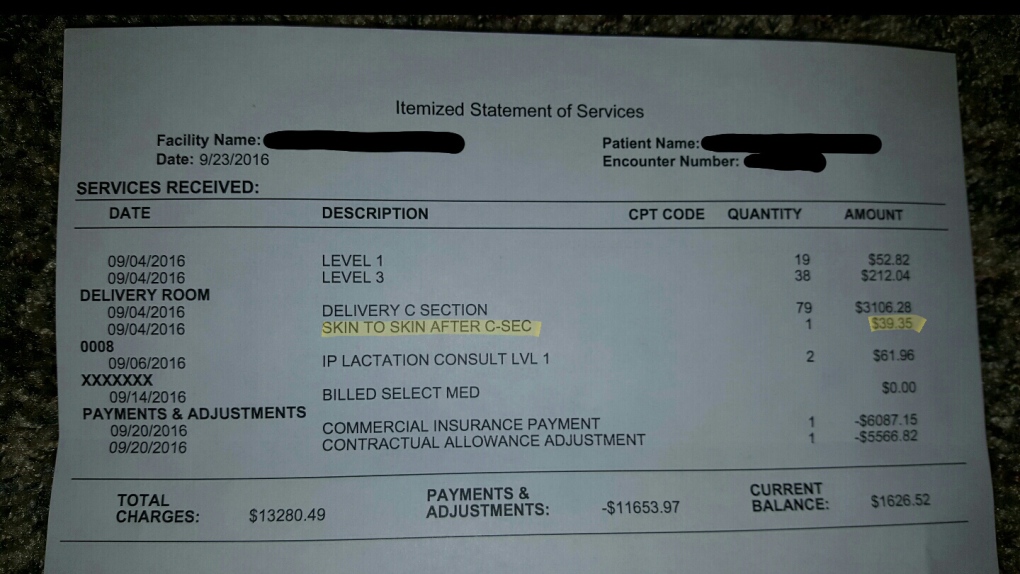
I remember that picture generated a lot of news, and even the explanation by a doula or hospital worker was insane
|
|
|
|
79 C-section deliveries seems like a lot to have in one day.
|
|
|
|
roomforthetuna posted:79 C-section deliveries seems like a lot to have in one day. There's no CPT codes on that for some reason but they're usually billed by time
|
|
|
|
roomforthetuna posted:79 C-section deliveries seems like a lot to have in one day. she sure must be tired!!!
|
|
|
|
Pittsburgh Fentanyl Cloud posted:There's no CPT codes on that for some reason but they're usually billed by time
|
|
|
|
roomforthetuna posted:That seems reasonable, though $39 per minute still seems like a lot, and delivering a bill that describes that as "quantity: 79" should be a crime. It can almost only be intentional obfuscation to make people compliant. If the bill had one unclear thing you might question it, but if literally the entire thing is completely inscrutable where do you even start? I suspect whoever posted that removed the CPT codes because they thought it was PII.
|
|
|
|
roomforthetuna posted:but if literally the entire thing is completely inscrutable where do you even start?
|
|
|
|
skooma512 posted:The only thing worse than getting a bill, is not getting a bill. Who knows if it's just sitting around on file waiting to go to collections? William Gibson, All Tomorrow's Parties posted:RYDELL'S father, dying of cancer, had told Rydell a story. He claimed to have gotten it from a book of famous last words, or if not famous then at least memorable.
|
|
|
|
Pittsburgh Fentanyl Cloud posted:I have a pretty good plan, we have no kids, and I'm paying $172.80 every two weeks for premiums. it's beyond parody. We've since moved to europe for work and my wife had to make a doctor's appointment before our heavily regulated but still boondoggle-light insurance is up and running. Which means she'll have to pay the uninsured rate out of pocket. 35 euro. and insurance will ret-con cover it because the hold up is the local immigration authority's fault. A friend who touches computers professionally was contracting for a while and the best plan he could find for his type-I diabetes-having-rear end and his wife & kid still had him paying over $300 month out of pocket just to keep himself alive with insulin and his cyborg pump-and-meter thing. But without insurance, he'd just...I dunno, die?
|
|
|
|
my gf started physical therapy to help with POTS a few months ago. her insurance wanted to stop covering sessions after just one month because they didn't think she was "improving" quickly enough it's all loving bullshit, some loving worm assigns a numerical value to your suffering and if it's costing them too much money they drop you
|
|
|
|
I took a look at their API on my insurance company's web site for responding to their inquiry. Responding with a “no” to other insurance is recorded as a “yes” if you later request the data back, and it’s not clear whether responding with a “no” to their request about Medicare eligibility is properly recorded. It seems to be in some places, but not others. It's literally impossible for me to submit a response in a way which will cause them to pay out a claim. And good loving luck to me in getting anybody to understand what the gently caress I'm talking about.
|
|
|
|
Went looking for a psychiatrist. Went to my insurer's website and called them to get a list of doctors who take my insurance. Called the doctors.... none of them took my insurance. They took cash patients though, $500 for the initial appointment and 200 (or so) for every appointment thereafter  . .In America, a psychiatrist is $700 dollars for treatment and may take weeks to see; however, a quality pistol is $500 and it's yours after 10 days. I guess it's because my insurance only covered treatments in house as I worked at a hospital. We had exactly one psychiatrist on staff. He didn't believe in medication and preferred to just talk to patients. He was so senile we had to reset his passwords literally every day. We brought it up to administration who kept him on because he was the only one and he doesn't prescribe meds anyway. That hospital went bankrupt and is now closed. Ended up going to my GF's psychiatrist who also just charged cash, but was cheaper and after an EKG and thyroid check, he doesn't hassle me and gives me generous allotments which he trusts me to manage on my own.
|
|
|
|
|
Griz posted:urgent care is for when you're uninsured and need antibiotics for an infected cut, or you think you have pneumonia or strep throat or something and it's not getting better on its own. i went to urgent care last night with a concussion and they said, despite being open, that they'd seen all the patients they could today. this is in chicagoland where covid isn't overwhelming hospitals so i went to the ER and my $500 copay wasn't charged because i'd already maxed out my nearly $3k out of pocket maximum from earlier this year
|
|
|
|
Kreeblah posted:I took a look at their API on my insurance company's web site for responding to their inquiry. Responding with a “no” to other insurance is recorded as a “yes” if you later request the data back, and it’s not clear whether responding with a “no” to their request about Medicare eligibility is properly recorded. It seems to be in some places, but not others. lol that's so they can deny and send you a letter asking you to verify that you have no other insurance. My insurerr five years ago did that to me even though I verified that I had no other insurance in response to a previous request. And I worked for them. You can verify and ask them to resubmit the claim but every layer of inconvenience makes it more likely you say 'gently caress it' and give up.
|
|
|
|
Pittsburgh Fentanyl Cloud posted:lol that's so they can deny and send you a letter asking you to verify that you have no other insurance. My insurerr five years ago did that to me even though I verified that I had no other insurance in response to a previous request. And I worked for them. That's exactly what they're trying to pull. They sent one of those letters and it arrived on September 9, but by that time, they'd already denied my claim the previous day for not responding to it. It's a claim for $93,282.44, so it's not like it's something I'm just gonna give up on (and, even if it was for something small, this sort of thing just pisses me off more).
|
|
|
|
I have good health insurance through my wife. They pay either 100% or 90% of everything and there's no deductible.
|
|
|
|
I have some do-nothing coverage where copays are outrageous but my monthly premiums are cheaper than the individual mandate that Biden's going to restore early next year. gently caress this country and everyone who supports it.
|
|
|
|
net work error posted:Health insurance companies loving suck so do giant hospital networks Northwestern University has been hellbent on becoming the sole hospital network in Illinois
|
|
|
|
a year or two ago i was working at a grocery store and my garbage rear end health plan was something ridiculous like 10% of my weekly check in a premium and also had a massive deductible. i don't know if that insurance ever paid for a single thing. then my teeth exploded and i had to get two pulled and a root canal and a bridge put in and it cost 4,000 dollars and dental doesn't come with health care. i put it on credit
|
|
|
|
two weeks ago we found out that my wife had miscarried, and she was far enough along that they had to do a d&c to get the remains of the baby out of her. we're obviously very sad, we had named the kid and everything. we are also stressed out waiting on the various bills we're going to get for this procedure, and also lol at mental healthcare, my wife's employee assistance plan will pay for i think 6 therapy sessions and then after that she's on her own. country fuckin sucks.
|
|
|
|
Cow Bell posted:a year or two ago i was working at a grocery store and my garbage rear end health plan was something ridiculous like 10% of my weekly check in a premium and also had a massive deductible. i don't know if that insurance ever paid for a single thing. In a sane world, the fact that there are people who pay a significant amount of their income every month for a plan which would bankrupt them before it paid out should be all the proof that anybody needs that this poo poo doesn't loving work. Of course, if we were in a sane world, we'd have a real healthcare system, so . . .
|
|
|
|
lobster shirt posted:two weeks ago we found out that my wife had miscarried, and she was far enough along that they had to do a d&c to get the remains of the baby out of her. we're obviously very sad, we had named the kid and everything. we are also stressed out waiting on the various bills we're going to get for this procedure, and also lol at mental healthcare, my wife's employee assistance plan will pay for i think 6 therapy sessions and then after that she's on her own. 
|
|
|
|
Text from a friend trying to file a claim
|
|
|
|

|
|
|
|
So I'm currently in a legal battle with Anthem. Last December, my work switched to UHC (lol), giving them ample notice, etc, that our plan was to be terminated on Dec01 2020. I have a few different med things going on that aren't super serious, but do require ongoing insurance-supported treatment. Think CPAP type stuff. I also take one particularly expensive biologic, so I have to constantly deal with making sure that's covered since I could never pay for a dose, let alone 4 a year. I alerted many of my providers that I was -going- to switch, but it took until late december to actually get insurance info from UHC. So, when I finally did, I gave the info to my providers and they started submitting claims. Tons of calls to offices, pharmacies, etc. Here's where it gets fun. Most of my providers did just fine, and started submitting claims. Unfortunately, around February 2021, I started getting a bunch of EOBs from UHC with declined services. Upon inspection, every single claim submitted from December 2020 to the present was declined due to "secondary insurance provider." It turns out that for months, Anthem had still been reporting that they were my primary insurance when doing coordination-of-benefits between UHC and themselves. Well, I had to get my HR at work involved, and after another 90 days after reporting this issue, Anthem finally managed to stop saying I was under their insurance policy. I had to then call back every single provider (who obviously had been hounding me for money) and tell them to resubmit every claim. They did, and after a time I finally had coverage and everyone got paid. Except for one. You see, on all my calls to providers, I had missed one office. It was a provider for medical equipment based on a proscription from a specialist. I let the doctor know but forgot to call the equipment provider directly. Well, they were in network 100% with Anthem, but were out of network with UHC. They sent me an automatic shipment in late december, then I got a bill. For out of network coverage. From Anthem. You know, the company that wasn't my insurance. Why had I gotten a shipment off of an expired insurance? It turns out that for this one claim out of dozens, Anthem for some reason paid the claim even though I wasn't covered, had no contract with them, and hadn't paid them anything for service in a month+ at that point. It wasn't a the world's largest bill, about $50, but I was flabbergasted. I started calling around to find out what had happened, etc. Finally after some nonsense, I had an anthem rep tell me directly, "Oh our system made a mistake, itll get covered, you shouldn't hear about this again." This was around April. Well, in June, I got another bill from the provider, same as before. I start contacting everyone, again, but at this point I have another weird concern: Anthem covered this provider 100%. They were in network. Why was I getting a bill at all if they had paid? Well it turned out that my plan didn't cover medical equipment 100% anymore. Anymore, you might ask? I asked this question myself, and apparently Anthem was billing me under the contract my company had declined to switch to UHC. Literally they billed me under a contract nobody had signed or paid for or agreed in any way to. Not only that, but they now claimed that because I wasn't actually covered, that they should in fact reclaim any money that they had paid to the provider. Again, for a shipment that wouldn't have been sent except that Anthem hosed up. They told my provider to bill me for the full (500+) dollar amount instead. For a shipment that should have never been sent except that Anthem randomly paid a claim they didn't cover. So, it's currently in the hands of the Virginia legal system. My bet is they're going to tell me to gently caress off (thanks Virginia) and have to rebill it to UHC, which are out of network and will charge me some amount. Absolutely insanely loving broken system we have in this country, and nobody that's had to interact with it in any real way can possibly think otherwise.
|
|
|
|
Oh and here's the biologic I couldn't possibly pay for
|
|
|
|
Skyl3lazer posted:Oh and here's the biologic I couldn't possibly pay for I'm speechless. What kind of business model turns a profit covering $23,200 of a $23,230 bill on a regular basis for one person?
|
|
|
|
Marx Headroom posted:I'm speechless. What kind of business model turns a profit covering $23,200 of a $23,230 bill on a regular basis for one person? Insurance companies get kickbacks from pharma companies for paying for certain drugs. So, say, the insurance company may pay $23,200 of that, then the manufacturer pays the insurer a $15,000 'rebate' for paying for the drug. The insurer may or may not share that rebate with the company that holds the policy.
|
|
|
|
Marx Headroom posted:I'm speechless. What kind of business model turns a profit covering $23,200 of a $23,230 bill on a regular basis for one person? god I hope I'm costing them money but I'm sure they find a way around it. I know, for instance, that the manufacturer has a copay assistance program which, depending on my insurance as it has changed, has paid between $5 and $5000 for each dose. I think it's literally a "see how much the insurance will give us, then we'll cover the rest" scam the drug company runs on the insurance ones.
|
|
|
|
just the usual fuckery for me, my insurance denied a claim so they're coming to me directly lmao gently caress off and talk to my insurance you were pre-approved submit the right loving billing code. if i'm really bored and feeling like my blood pressure is extra low sometime i'll deal with it.
|
|
|
Harik posted:just the usual fuckery for me, my insurance denied a claim so they're coming to me directly lmao Hope you have some sweet games to play while on hold for 2 hours.
|
|
|
|
|
Their Baby Died in the Hospital. Then Came the $257,000 Bill.quote:Last summer, Ms. Lane started receiving debt collection notices. The letters, sent by the health plan Cigna, said she owed the insurer over $257,000 for the bills it accidentally covered for Alexandra’s care after Ms. Lane switched health insurers.
|
|
|
|
https://mattstoller.substack.com/p/the-villains-behind-our-medical-supply "The Corrupt System Behind Covid Medical Shortages Why are we still facing shortages of masks and medicine a year and a half after the start of the pandemic? Because a buying cartel controls medical supplies, and has for 25 years."
|
|
|
|
|
skooma512 posted:https://mattstoller.substack.com/p/the-villains-behind-our-medical-supply Proclick
|
|
|
|
https://www.fox5atlanta.com/news/woman-billed-700-after-sitting-in-er-waiting-room-for-7-hours-leaving-without-treatment ATLANTA - A woman said she was billed for a trip to the emergency room, even though she didn't receive any treatment. Taylor Davis said she went to the Emory Decatur Hospital ER in July for a head injury. She sat in the waiting room for hours, but with no end in sight, she decided to leave. "I sat there for seven hours. There's no way I should be sitting in an emergency room.. an emergency room for seven hours," she said. A couple of weeks later, a surprise came in her mailbox. It was a bill from the hospital for nearly $700. "I didn't get my vitals taken, nobody called my name. I wasn't seen at all," Davis said. Davis said she was convinced it was a mistake. "So I called them and she said it's hospital protocol even if you're just walking in and you're not seen. When you type in your social, that's it. You're going to get charged regardless," she said. She said she was told it was an emergency room visit fee or a facility fee as it is called in some cases. It's often added to a person's total hospital bill, so it might not be as noticeable as it is in this case. An email sent to Davis by an Emory Healthcare patient financial services employee states "You get charged before you are seen. Not for being seen." Davis said unfortunately, she'll think twice before stepping foot in an ER., now that she knows what she can potentially be charged with, "I'm very reluctant to go to the hospital now. That's kind of like the last resort now. Seeing that they're able to bill you for random things, it doesn't make me want to go. So that's not good," Davis said. Emory Healthcare sent the following statement: "Emory Healthcare takes all patient concerns seriously and appreciates this has been brought to our attention. Our teams are currently looking into this matter and will follow up directly with the individual." Eroding faith in the healthcare system and getting some fraud in for good measure.
|
|
|
|
|

|
| # ? May 5, 2024 07:15 |
|
Thinking about that time I got a kidney stone in the 00s and didn't have insurance or anything and had to go to the ER and got an ultrasound and ultimately an IV of ibuprofen and they sent a bill that was $100,000 but its ok there was an "uninsured discount" down to only $50,000 i love that some of the best advice i can give for dealing with medical insurance is "you probably can just like not pay them if you don't care about your credit score" and honestly everything is so bad medical debt doesn't ding your score as much as it used to anyway thankfully i haven't had any big disasters in recent years but i have kaiser and they just kind of randomly have bills that i don't even see most of the time and my ex-wife who doesn't live in reality would scream incoherently about and is now trying to claim she paid even though i have my doubts. even in kaiser's closed system it's hard to get a straight answer what the gently caress anything is for. i currently owe them like $1600 and gently caress if i could tell you why. i think its out of pocket maximums. maybe. who knows. regretfully i have to care about my credit score right now so i am paying it despite being very objected to it. i just want to go look at the bill and it doesnt make a lot of sense, i think i hit some sort of out of pocket maximum for an expensive drug im on but none of this is obviated at all and is very confusing for it being a very straightforward deal of "i take one expensive medicine". also it is common for these plans to still make you pay double digit percentages of expensive specialty drugs. and i have a good office worker plan and it still has poo poo like "well you might have to pay up to $3000 a year for bullshit" like cool i just have that in my back pocket. but now i have to navigate getting my own kaiser through my new job where despite having contracted here since february i was only recently converted but dont actually get to have insurance until the beginning of next year so that is really neat. it seems to have a lot of dumb rules because they seem to have a wacky deal with them for various reasons i can only speculate that involves there being different services and pharmacies than i would expect from kaiser so i am looking forward to dealing with that.
|
|
|